Welcome to AOE’s October 2024 edition of AOE Compliance Connection, our monthly newsletter. As we work our way into fall, the CE community is brimming with announcements, activities, and growth opportunities. AOE is poised to help you and your team take on the next challenge: Don’t hesitate to reach out to us with questions of any kind. This month’s newsletter will brief you on the recent WFME announcement about their new recognition for CPD providers, a host of ACCME updates including content tagging and annual fees, and Medicaid regulation updates that may be relevant to you and your learners.
Take a moment to ensure you’re following us on social media so you don’t miss helpful weekly tips and compliance updates!

International CE: Global Recognition Program for CPD Providers
AOE frequently fields questions from accredited providers regarding ACCME and international accreditation board requirements. The World Federation for Medical Education (WFME) is part of that response. The WFME’s view of that one benefit of CPD in general is that it provides a “robust framework for borderless education”.
Recently, the WFME announced a new global recognition program for CPD accrediting agencies, inclusive of ACCME-accredited providers. In the months to come, WFME plans to establish a “Recognition Committee”, finalize their criteria, and train staff appropriately. There will be a detailed application process online soon for any accrediting agencies seeking recognition and will also display the accrediting agencies that have achieved the recognition.
ACCME President and CEO Graham McMahon, MD, MMSc, expressed that the “ACCME is delighted to see the international standards we jointly created be utilized by WFME to create a global system of recognizing high quality CPD accreditation systems. This will help licensing authorities around the world decide which CPD credits to accept as legitimate, which will be invaluable in creating quality learning experiences for healthcare professionals.”
WFME, a non-governmental agency, was founded in 1972 and since then has served as an international platform for “harmonizing principles and standards across the entire spectrum of medical education”. They now recognize 47 agencies and aim to continually set new benchmarks in CPD for physicians, making sure that medical professionals remain informed and equipped.
Read more about the WFME’s new CPD recognition program here.

ACCME Compliance Support: Three Reminders
We’d like to share with our readers three helpful tips from the online world of ACCME that could help your team this month:
Annual Accreditation Fees
 ACCME Accredited providers will be receiving their invoices on or before October 22, 2024, via email. (Payment is due by January 31, 2025). Make sure your contact information in PARS is updated and current to ensure you receive the invoice.
ACCME Accredited providers will be receiving their invoices on or before October 22, 2024, via email. (Payment is due by January 31, 2025). Make sure your contact information in PARS is updated and current to ensure you receive the invoice.
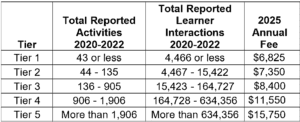
These fees will reflect the new tiered structure and are represented in this ACCME table:
Content Tagging in PARS
One of the recent updates to PARS in a newly enabled option that allowed providers to tag activities specifically for physicians with pain management-related state medical board licensing requirements. In the future, the ACCME aims to support broader tagging of content (ideally through AI) related to state licensing to ultimately aid physicians in identifying relevant educational initiatives specific to the Medication Access and Training Expansion (MATE) Act. The MATE Act requires specific training for medical professionals who prescribe controlled substances. At this time, providers can access this optional feature via the web form in PARS and can expect future educational webinar series with clear instructions.
Thinking Ahead to Annual Reporting
As we enter quarter 4 of the business year, it’s a good time to begin thinking about annual reporting. The ACCME encourages providers to use PARS to close activity records when the activity ends and to submit learner credit data (not to wait until year’s end!). Doing this regularly gives you a head start on completing your annual learning requirements.
As per usual, March 31 will be the deadline for completion of the Program Summary and Annual Agreement and closure for all activities that ended in the prior year. The sooner providers finish entering and closing 2024 activities, the faster they’ll be able to complete annual reporting requirements come January.
Read more about the requirements and steps for annual reporting here.

CE Community: Updated Medicaid Regulations
The Centers for Medicare & Medicaid Services (CMS) recently published two Medicaid regulations: 1) a Medicaid Access Rule and 2) a Medicaid Managed Care Rule. Both updates introduce new requirements for states and Medicaid care plans that will “enhance and standardize reporting, monitoring, and evaluation” of Medicaid access to services.
Tom Sullivan, on the Policy and Medicine website, concludes that “ultimately, these rules will significantly increase transparency for Medicaid and CHIP program data related to provider payments and access to care. States and managed care plans must soon begin publishing several new types of data sets and reports, which must be publicly available in a standardized format and with relevant context.” He also cites the consistency in the CMS’s continued focus on health disparities and equity and the HHS’s continued prioritization of closing those same gaps.
Medicaid Access Rule:
Among other things, the Medicaid Access Rule:
- Creates new transparency and consultation requirements for FFS (fee-for-service) provider payment rates
- Includes a state requirement for publishing analyses comparing FFS rates between Medicaid and Medicare
- Aims to establish a “interested parties’ advisory group” to advise on HCBS payment rates
- Includes new procedural requirements for FFS rate changes
- Strengthens program advisory groups through creation of MAC and BAC committees
- Updates HCBS program standards and processes
Medicaid Managed Care Rule
Among other things, the Medicaid Managed Care Rule:
- Improves access to care and monitoring requirements in manage care programs
- Establishes federal minimum standards for appointment wait times
- Enhances state requirements for access monitoring
- Requires states to publish analyses of some provider payments
- Revises federal regulations surrounding SDPs
- Builds on recent CMS policy changes about ILOS
- Modifies MLR methodologies and processes
- Establishes a national framework for QRS
Find information about the Medicaid Access Rule here, and about the Medicaid Managed Care Rule here.
Upcoming Events
- Learn to Thrive PLUS
October 29, 2024, Virtual Live
Read More >> - ANCC NCPD Summit
October 28-29, 2024, New Orleans, LA
Read More >> - ANA 2024 National MagPath Conference
October 30-November 1, 2024, New Orleans, LA
Read More >> - MAACME 2024 Annual Conference
November 12-13, 2024, Blue Bell, PA
Read More >> - ACPE CPE Provider Conference
November 18-20, 2024, Chicago, IL
Read More >>








